So what’s happening? What is the connection between food allergy (and sensitivity) and depression? To answer this question, we need to understand what happens in the brain when at least some forms of depression occur.
I need to make a disclaimer here. I am by no means an expert in this field. I’m learning as I go and will just give you the outline of what I think is happening, fleshing it out later as my research progresses. I do have a Bachelor’s degree in Microbiology that I received from UC Santa Barbara in 1990 and I worked for 8 years as a molecular biologist, for what it’s worth.
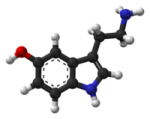
Depression, as well as a number of other ailments, have been linked to low serotonin levels. Serotonin is a neurotransmitter, also called 5-HT, and is synthesized within the body from the amino acid tryptophan (trp) which we get from the protein that we eat. We always have a certain level of trp in our blood, circulating around, but when something happens to cause trp levels to decrease, there is less available trp for our bodies to make 5-HT. It has been shown that in chronic infections such as HIV or hepatitis C, there are low levels of trp in the blood and patients with HIV or Hep C will also have neurological disorders such as depression. (Christmas DM, Potokar J, Davies SJ. A biological pathway linking inflammation and depression: activation of indoleamine 2,3- dioxygenase. Neuropsychiatr Dis Treat. 2011;7:431-9) Why would this happen? Because there is an enzyme that is produced in the body by certain cells of the immune system, specifically by mast cells and dendritic cells. This enzyme is called indoleamine 2,3-dioxygenase (IDO) and its function is to metabolize tryptophan. It’s part of the body’s defense mechanism…to rob invading pathogens of the resources (i.e. trp) they need to replicate as well as to regulate T-cells, a very important component of the immune system. The problem is, when you have an illness that leads to chronic inflammation, this IDO is turned on all the time, depleting the tissues of trp and therefore causing a low level of serotonin the brain which in turn, leads to depression (ibid.). Another contributing factor is the catabolism of tryptophan by IDO creates byproducts that are neurotoxins and this may also cause neurological disease. In my own experience, however, I tend to think it’s more of the former (a topic for another day), although both scenarios likely play a role.
How is this connected to food allergy and sensitivity? I haven’t found any published research to support my theory, but I think it makes sense to say that if the body is constantly exposed to food allergens in the gut, there is going to be a certain level of chronic inflammation and consequently excessive and prolonged IDO production, which over time can lead to trp depletion. There is also the fact that 95% of the body’s serotonin receptors lie not in the central nervous system, but in the gut! The role serotonin plays here is gut motility. The gut contracts around food, moving it along as serotonin is released by certain cells lining the gut. If irritated, more serotonin is released and diarrhea occurs and if enough serotonin is released that it raises serotonin levels in the blood, vomiting will occur. In addition to the action of IDO, I wonder if levels of trp are depleted by the synthesis of serotonin during episodes of intestinal illness and the inability of the sick person to eat enough protein to replenish trp levels.
I think any inflammatory diet can lead to depression, but perhaps it may be more pronounced with allergies and sensitivities. To quote the above article,
“Emerging evidence demonstrates that: a) major depression is associated with increased inflammatory drive;1-3 and b) provoking an acute inflammatory response in healthy humans can result in depression-like behaviors and symptoms.4-5″
According to a 2011 Gallup-Healthways Well-Being Index™ survey, 40 million Americans suffer from depression. And according to a CDC report, also from 2011, 1 in 10 Americans take antidepressants, with a comment that about 1/3 of those with severe depression do not take prescription medication. SSRIs, or selective serotonin re-uptake inhibitor, in the class of medication most widely prescribe for depression.
So what does this mean? That if you can find the food trigger in your diet that is causing your body to suffer from chronic inflammation, you may be able to recover from depression and stop taking daily medication. It worked for me. When I stopped eating gluten and dairy, my depression ceased. My anxiety vanished. I’m not allergic to wheat, but I do have a sensitivity to gluten. I also was allergic to dairy when I was a young child, and my symptoms went away around the age of 8, but I know that I am still sensitive to it. It may not be gluten and dairy for you. It might be something else, like corn or soy. Maybe it could be a diet high in processed foods. But considering that eliminating one or two kinds of food is certainly a more desirable choice than taking antidepressants or anti-anxiety pills every day, why wouldn’t you take the first step and get tested for food allergies? If you’re not allergic to any foods, why not start a food journal and record what you eat and how you feel, then start eliminating suspect foods from your diet for a month or two? How many people suffer in this world from unexplained depression and how many of those people have undiagnosed food allergies or sensitivities? How many of those could be CURED of that suffering if they only eliminated the foods they shouldn’t be eating in the first place?
One last note. The research links low levels of serotonin based on IDO activity to depression only and not anxiety. While the standard medical treatment for depression differs from anxiety, it is known that there is a link between the two disorders as people with depression also often suffer from anxiety. In my case, I had both as well, and in searching for a cure for anxiety, I also cured my depression. And it was all linked to the diet I was eating.
References:
1. Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009; 71(12): 171-186
2. Kim YK, Na KS, Shin KH, Jung HY, Choi SH, Kim JB. Cytokine imbalance in the pathophysiology of major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007; 31(5): 1044-1053
3. Maes M, Bosmans E, Meltzer HY. Immunoendocrine aspects of major depression. Relationships between plasma interleukin-6 and soluble interleukin-2 receptor, prolactin and cortisol. Eur Arch Psychiatry Clin Neurosci. 1995; 245(3): 172-178
4. Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR. Inflammation and social experience: an inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain Behav Immun. 2010;24(4): 558-563
5. Reichenberg A, Yimmiya R, Schuld A, et al. Cytokine-associated emotional and cognitive disturbances in humans. Arch Gen Psychiatry. 2001;585(5): 445-452
Categories: Theory
Great article Ami! Very interesting.. I wonder then if daily suppplemental tryptophan would be another way to help treat depression . Thanks.
Hi Jo Ann, thanks for the comment. Certainly supplemental tryptophan can help. I’ve taken OTC 5-HTP and had it help me. But I’d like to focus on curing the disease and not treating the symptoms. I’m slowly trying to get my story out there and explain what I think is going on is curable, for some people, by simply eliminating foods they react to that causes inflammation. I’m going to have to get to work on another post today!
This is wonderful. Thanks for stepping up and putting this out. Your efforts and knowledge are valuable. I hope this helps others become aware of how far reaching daily nutrition is for our lives, bodies, and minds. Keep it up.
Hi Jesse,
Thanks for looking at my new blog! There’s not much there yet, but I have high hopes. Pass it along to your friends.
Changed my diet completely depression and anxiety still very much with me starting to loose hope
I’m sorry, I didn’t see this post until recently. We were in the process of a major move when you wrote and somehow missed it. How have you changed your diet and when? Do you know if you’re allergic to anything and have you sought medical help? I started this blog to help people whose allergies may be caused by food, but I want to be clear. While I believe some allergies cause depression and anxiety, I don’t believe all causes of depression and anxiety are food based. There are many other possibilities and I hope you try every means available to you in order to control or cure your depression and anxiety. I wish you the best.
Just back from my Environmental Medicine doc where I had some skin testing to see what can be done for my chemical sensitivities. It turns out I am highly allergic to serotonin! I am taking drops to desensitize, and am wondering how this relates to longstanding battles with depression. I have many food allergies. I think chronic inflammation is a problem. Very interesting!
Amy
I was searching (seratonin allergy). Like you I think there is a connection. I have discovered through research that 5-HTP does help significantly with my chronic lung inflammation. I also ran across this link. I think you will find it very interesting and I would say my results are the same.
Thanks Greg! I’ll take a look at it. 5-HTP can help replenish serotonin levels, but I’d be concerned about the underlying cause of the inflammation. If IDO is metabolizing tryptophan and subsequently causing a serotonin deficiency, certainly 5-HTP can help mitigate those symptoms associated with low serotonin levels. I’ve experienced this myself after a bout of stomach flu and migraine that left me craving only carbs for the better part of a week. Then like a wave crashing, I had an anxiety attack. Realizing I had very little protein to eat that week, I took 5-HTP, ate beef jerky and pumpkin seeds and within 20 minutes all symptoms had cleared.
However, what I would be concerned about is chronic inflammation and treating the symptoms solely with 5-HTP. I’m sure you’ve come across references citing the byproducts of IDO metabolism of tryptophan are neurotoxic, namely 3-hydroxykynurenine, 3-hydroxyanthranilic acid and quinolinic acid. An imbalance in the Kynurenine pathway could also perhaps cause anxiety and/or depression. It’s certainly implicated in other neurodegenerative diseases. Dr. Emily Deans has posted a very good explanation of the biochemical and neurotoxic effects of tryp metabolism, but I could not find the link doing a quick search.
Thanks again!
This is a great article. I am a strong believer that all disease begins in the gut. I have been doing a lot of research on digestive issues. Your explanation is very informative.
Have you considered glutamates? Some people have genetics that lend them to vulnerabilities of glutamate sensitivity. Not a food allergy necessarily.